Dementia & Alzheimer’s: A Plainspoken Overview with Real-life Examples
- May 30, 2025
- 10 min read
Updated: Aug 11, 2025

My grandmother had dementia (likely Alzheimer's). My mom just passed away from Alzheimer’s a few weeks ago. I’ve barely processed the whirlwind that was the last 2 years for her, for all of us.
As Mom was battling the disease, I did what I always tend to do, I started researching. I wanted to understand what was happening to her brain. Why it was happening. How it usually progresses. And why it doesn’t always follow a script.
Along the way, I’ve learned a lot — about the different types of dementia, how early it can start, how Alzheimer’s unfolds in stages, and mixed dementia (like my mom had) can complicate the picture.
This post is not a clinical deep-dive. It’s the version I wish I had early on — a plainspoken overview of what dementia and Alzheimer’s is, and how it looked for us.
Dementia vs. Alzheimer’s: What’s the Difference?
When someone starts forgetting things more often or acting differently, we often wonder if it’s normal aging or if it might be dementia. Occasional forgetfulness — like misplacing your keys or forgetting the name of an actor on TV— is common as we age. Dementia involves more persistent, disruptive changes that begin to interfere with everyday life and relationships. While memory loss is the most well-known symptom, dementia can also affect problem-solving, behavior, communication, and even physical coordination.

Dementia isn’t a specific disease — Dementia is an umbrella term for many different types of cognitive disease, including (but not limited to):
Alzheimer’s disease – the most common type, affecting 60–80% of cases
Vascular dementia – often caused by reduced blood flow to the brain
Lewy body dementia – may include movement issues and visual hallucinations
Frontotemporal dementia – typically affects language, judgment, and behavior
Mixed dementia – when two or more types occur together (as in my mom’s case, which combined Alzheimer’s and vascular)
Each type has its own path, symptoms, and progression. That’s why everyone’s journey with dementia can look so different. What shows up early for one person may not show up at all for another.
✦ ✦ ✦ ✦ ✦
—In my mom’s case, the changes felt sudden to the rest of us — but looking back, we think my dad had been quietly covering for her for quite some time. Not intentionally. He just didn’t recognize it for what it was. He filled in the blanks when she forgot things. Steered conversations when she got confused. Managed routines so that the cracks didn’t show.
When it became undeniably clear that something wasn’t right, he convinced her they should move into assisted living — framing it as something he needed for his own physical limitations. That was his way of protecting her dignity. It was also the beginning of a very different chapter.—
It Starts Sooner Than You Think
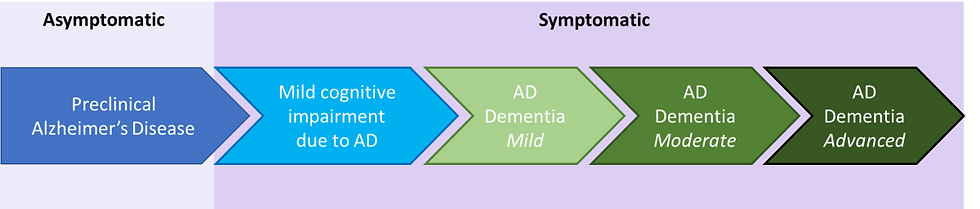
One of the most startling things I’ve learned is how early Alzheimer’s can begin — not the symptoms we see on the surface, but the changes happening deep inside the brain.
I was stunned to learn that Alzheimer’s can simmer under the surface for decades— 10 to 20 years (or longer)— before symptoms show up.
During this quiet phase, abnormal proteins like beta-amyloid begin to build up, and damage to brain cells slowly starts to take hold. But there are no obvious warning signs — nothing that would make you think this is the start of Alzheimer’s.

By the time memory issues or confusion show up, the brain may have already been under attack for years. This is also why prevention matters — long before symptoms ever appear. And just because you carry a gene such as ApoE4, it doesn’t mean Alzheimer’s is inevitable. Functional health experts often say: “Genetics loads the gun, but environment pulls the trigger.” Your DNA is not your destiny – daily choices still matter. If you haven’t read my article about Brain Health & ApoE4, you may want to check that out as well for more insight on the genetic link.
✦ ✦ ✦ ✦ ✦
—For my mom, the earliest signs were subtle but persistent. She started asking the same question over and over — not out of distraction, but because she truly didn’t remember already asking it. She began struggling with routine tasks, like balancing the checkbook and grocery shopping. At one point, we found 15 large containers of broth and 10 cans of beans stacked in her pantry — she kept buying them because she forgot that she had done so on the last trip.
Then came the daily trips to HomeGoods — and I do mean daily. She’d ask to go every single day, and when she did, she almost always came home with the same things: small plastic plants, decorative boxes, and throw pillows. At one point, she had at least 50 faux plants and dozens upon dozens of pillows tucked around the house. HomeGoods wasn’t just her happy place — it became her daily ritual.
She also started wandering the house at night — restless, unsure of time or place. At first, Dad just rolled his eyes and didn’t think much of it. But eventually, it was clear something much deeper was happening.—
The Stats: So How Widespread Is Alzheimer’s?
Alzheimer’s isn’t just a personal or family issue — it’s a growing public health crisis.
In 2025, an estimated 7.2 million Americans aged 65 and older are living with Alzheimer’s disease. That’s about 1 in 9 people over 65!
By 2050, that number is projected to nearly double, approximately 13.8 million.
Almost two-thirds of Americans with Alzheimer’s are women.
Black Americans are about twice as likely, and Hispanic Americans about 1.5 times as likely, to develop Alzheimer’s compared to older white adults.
The cost of care is projected to reach $384 billion in 2025, and nearly $1 trillion by 2050.
📊 Source: Alzheimer’s Association, 2024 Alzheimer’s Disease Facts and Figures

The Stages of Alzheimer’s: A General Guide
Alzheimer’s doesn’t progress the same way for everyone — but most experts divide the disease into three general stages: Mild, Moderate, and Severe. Some models break it down further (7 stages), but for the sake of clarity, we’ll keep it high-level here.
🕰️ How long does each stage last?
It really varies. Some people move through the stages in just a few years; others live with Alzheimer’s for a decade or more. What you’ll see below reflects the typical, but remember Alzheimer’s doesn’t follow a script.
🟢 Mild Alzheimer's Disease (Early Stage)
Typical Duration: 2–4 years
Cognitive Equivalent: ~10–12 years old
What You Might Notice:
Asking the same question repeatedly— often within minutes
Subtle memory lapses (missing appointments, forgetting names)
Trouble with planning or multi-step tasks (balancing a checkbook)
Giving up familiar routines (my mom stopped cooking altogether — baking had always brought her joy)
Word-finding issues and getting flustered mid-sentence
Mood changes, especially defensiveness or denial
At this stage, people may still seem “mostly fine” to others — but those closest start to see the small cracks. It’s also the point when many families begin walking on eggshells, unsure how to help without triggering fear or frustration.
🟡 Moderate Alzheimer's (Middle Stage)
Typical Duration: 3–6 years
Cognitive Equivalent: ~4–7 years old
What You Might Notice:
Getting lost — even on familiar routes
✦ ✦ ✦ ✦ ✦
—Mom had an episode late in the Mild stage, when she got lost driving home from the grocery store. It terrified her. She never drove again after that. It was also the moment my dad started thinking about assisted living. When in the Moderate stage, she would get lost getting back to her room after dining, and hated elevators because they completely disoriented her.—
Difficulty using everyday items like phones or TV remotes
Forgetting close family members’ names or confusing relationships
Increased paranoia (often thinking people are stealing from them)
Delusions and hallucinations
✦ ✦ ✦ ✦ ✦
—Mom insisted kids were running up and down the halls all night. She once claimed that she was given half of a ham sandwich for dinner while “the fat cats were partying upstairs, eating lobster!” And one of the worst was when she “saw” a large man with a hammer, smashing things in her room.—
Loss of interest in hygiene or changing clothes
Major personality shifts — angry, agitated, suspicious
This was the hardest stage for our family. She was miserable — and so were we. There were tender moments, of course, but they were buried under layers of confusion, fear, and heartbreak.
🔴 Severe Alzheimer's (Late Stage)
Typical Duration: 1–3 years
Cognitive Equivalent: ~infant to toddler level
What You Might Notice:
Severe memory loss and confusion
Speech becomes almost non-existent
✦ ✦ ✦ ✦ ✦
—In my mom’s case, she could barely get a sentence out, and when she did, it was often jumbled or nonsensical. In her final week, she couldn’t speak at all. —
Changes in movement — some people lose mobility entirely or transition to wheelchairs.
Needing help with all daily tasks — bathing, dressing, toileting
Difficulty eating or swallowing — though my mom didn’t experience this until her final week, many in this stage require help feeding for quite some time
Sleeping much of the day, with occasional moments of alertness or emotional connection
By this point, the disease has robbed so much. But even here, connection isn’t impossible. There were moments — brief, beautiful ones — when I still felt her presence. A look, a touch, something in her eyes that said, “I know you.”
✦ ✦ ✦ ✦ ✦
—For my mom, the “late stage” lasted barely a month. Her entire journey — from diagnosis to passing — unfolded over just 14 months. Note: that kind of fast progression is not typical. Mom had nearly every known factor that can accelerate decline.—
What Can Speed Up Alzheimer’s Progression?

There’s no single reason why Alzheimer’s speeds up in some people and moves more slowly in others — but researchers and caregivers alike have identified several common contributors. These factors can interact in complex ways, especially when they overlap.
🩺 Vascular Risk Factors
Untreated high blood pressure, heart disease, stroke, diabetes, and high cholesterol are strongly associated with a faster rate of decline.
✦ ✦ ✦ ✦ ✦
—In my mom’s case: she had a history of high blood pressure, and we later saw evidence of small vein ischemic disease (SVID) on her MRI which is basically damage to tiny blood vessels in the brain leading to reduced blood flow. Either of these things (or both) likely compounded the progression.—
🧠 Brain Injury
Injuries to the brain — from falls, concussions, or strokes — can worsen dementia symptoms or accelerate decline.
✦ ✦ ✦ ✦ ✦
—My mom had multiple falls, including a few with head trauma. Each one seemed to chip away at her stability. The last one resulted in a brain bleed which would ultimately end her life. —
⚠️ Stressful Life Events
Emotional shocks and life stress — including the death of a loved one — can lead to sudden or sharp declines.
✦ ✦ ✦ ✦ ✦
—My dad passed away unexpectedly just before they were to move into assisted living together. That emotional trauma was devastating for her.—
🔄 Changes in Routine
Transitions like moving homes, switching care facilities, hospitalization, or having unfamiliar caregivers can cause disorientation or behavioral setbacks.
✦ ✦ ✦ ✦ ✦
—In a short span of time, Mom moved from her home of 30+ years into a small villa with Dad, then to assisted living (without Dad), then to Memory Care (including a change in facilities). Too much for most people, way too much for anyone battling Alzheimer's. It was never our intention to trigger more trauma. We didn't foresee Dad passing when he did; add a combination of life circumstances and desire for the best care possible... it was what it was. —
🏥 Medical Complications
Hospital delirium, unmanaged infections, or certain medications can worsen symptoms — sometimes permanently.
✦ ✦ ✦ ✦ ✦
—While not a major factor for Mom, this is something we watched closely during her care.—
🧍♀️ Sedentary or Isolated Lifestyle
A lack of physical activity, social interaction, or cognitive stimulation can accelerate cognitive decline.
✦ ✦ ✦ ✦ ✦
—Mom’s world grew smaller after Dad passed, and as her disease progressed she became increasingly sedentary.—
🧬 Genetic Vulnerability
Carrying one or more copies of the ApoE4 gene variant — like I do — can increase risk and may also speed up progression by making brain cells more vulnerable to tau and amyloid buildup.
✦ ✦ ✦ ✦ ✦
—We don’t know if Mom had this gene variant, it was never tested to my knowledge. Given her mother had dementia, and she was diagnosed with Alzheimer’s, and I have the ApoE4 variant, I’m guessing that I got my one copy from her.—
🔗 Mixed Dementia
This term refers to having more than one type of dementia at the same time—most commonly, Alzheimer’s combined with vascular damage. When Alzheimer’s and vascular dementia show up together, the resulting progression is faster, more chaotic, and harder to treat. The symptoms are more severe and unpredictable. Some days they can string together a thought. Other days, reality is completely out of reach.
✦ ✦ ✦ ✦ ✦
—And yes, my mom had Mixed Dementia too (Alzheimer's & Vascular).
In many ways she experienced a “perfect storm” — a worst-case scenario. While each of these accelerating factors on their own can be manageable, together they created a very rapid and heartbreaking decline.—
Coming Up
Alzheimer’s is hard to understand from the outside — and even harder to live through. If you’re reading this because someone you love is going through it, I hope this gives you a bit of clarity, validation, or even words for something you’ve seen but struggled to explain.
This isn’t the end of the conversation — I’ll be writing more on related topics like:
Choosing a Memory Care Facility
Wasted Time & Money: The Faulty Alzheimer’s Research We Trusted Too Long — what we focused on, what we missed, and what we now know (a follow-up to my ApoE4 article)
Can You Prevent Alzheimer’s? What the latest science says about diet, exercise, ApoE4, and beyond
The Caregiver Experience — the emotional toll, the guilt, the moments of beauty, and the burnout no one prepares you for
If you’re walking this path, you’re not alone.
If you are worried about cognitive decline, take heart in learning there is much we can do to improve our brain health… (hint: a big part is reducing inflammation). Remember that changes in our brains start happening long before noticeable symptoms (sometimes decades!), so be proactive. I wish I knew when I was in my 40s so that I could have started some of the things I'm doing now much sooner... but it's not too late my 60-somethings. I started my brain-health journey 3 years ago and I continue to level up as I go!
Stay curious, friends.

💡TIP on COMMENT BOX BELOW: "Email" is optional - just type your Comment and Publish.
Comments